With over 17,000 cases and 52 case reports to date, DermaClose has the real world proof you need
Ortho/trauma surgery
60-year-old male with traumatic open ankle fracture and history of two failed rounds of NPWT
Presentation: 60 year-old male patient presented with a traumatic open ankle fracture and history of two prior failed rounds of Negative Pressure Wound Therapy (NPWT or V.A.C).
Size of wound: 7” x 5”, the wound had been open for 14 days prior to intervention
Time to closure: 5 days
Vac use: No
Outcome: Examination 7 weeks later revealed a stable, closed wound.
.
40-year-old male with necrotizing fasciitis
Presentation: A 40-year-old male was treated with DermaClose for a 40 cm x 12 cm wound caused by necrotizing fasciitis. He was initially treated with surgical debridement and negative pressure wound therapy (NPWT, or VAC) to help stabilize the wound and prepare it for closure.
Size of wound: 40 cm x 12 cm, two medial bypass sites were 10 cm x 6 cm
Time to closure: 9 days
Vac use: Yes
Outcome: 2 months after removal of DermaClose, the wound has healed very well. I would not hesitate to use and recommend DermaClose for similar appropriate procedures.
Photos courtesy of Neil R. MacIntyre III, MD
Young patient with large, avulsion injury
Injury: Avulsion of the left leg
Surgeon: Dr. Neil R. MacIntyre III, M.D.
Patient: 8-year-old male
Presentation: Patient presents with an avulsion injury of the left leg. Prior to DermaClose he received operative washout, an external fixture, and application of VAC.
Size of wound: 15 cm x 8 cm
Time to closure: 5 days
Vac use: Yes
Outcome: 9 weeks later the external fixture was removed and the leg was casted with a window for monitoring and care of the would. There were no issues with infection.
Photos courtesy of Wadih S. Macksoud, MD
Injury: Above the knee amputation of the left leg
Surgeon: Dr. Wadih S. Macksoud, MD
Patient: 14-year old male
Presentation: Patient presents with injuries unstained as result of getting caught in a boat propeller. He underwent an above the knee amputation of the left leg and an achilles tendon repair on the right and a rotation fasciocutaneus flap used to cover tendon due to missing overlying skin.
Size of wound: Unknown
Time to closure: 7 days
Vac use: No
Outcome: The tendon healed without complication and the patient started weight bearing on day 30. He was fitted for a prosthetic and continues to progress nicely.
Photos courtesy of Ajul Shah, MD
Injury: Necrotic infected carpus, loss of multiple fingers, and loss of soft tissue domain on dorsal forearm and dorsal hand.
Patient: 46-year old female
Presentation: Patient carried severe medical comorbidities including end-stage renal disease and type 2 diabetes. It was determined that salvage of the upper extremity would not be feasible or possible, and therefore, transradial amputation was recommended.
Size of Wound: Unknown
Outcome: At 2 weeks post-operative, the wound completely healed. Patient completed rehabilitation for integrated of targeted muscle reinnervation and received a myoelectric prosthesis. The durable soft tissue reconstruction allowed for pain-free utility of the myoelectric prosthetic without concerns for skin breakdown.
Photos courtesy of Ajul Shah, MD
Injury: Avulsion injury of the left upper extremity at the level of the proximal humerus.
Patient: 47-year old male.
Presentation: Patient was at the trauma center with a complete shoulder disarticulation procedure. Patient was transferred to the reconstructive surgery service. Tissue expansion and target reinnervation was performed.
Size of Wound: Unknown.
Outcome: Sutures were removed after 2 weeks post-operative. Wounds were completely healed. Patient was integrated into an amputation reconstruction program. Rehabilitation was completed and the patient received a myoelectric prosthetic.
Photos courtesy of Ajul Shah, MD
47-year-old diagnosed with severe compartment syndrome syndrome with ongoing rhabdomyolysis
Injury: Severe compartment syndrome with ongoing rhabdomyolysis. Patient was taken to the operating room for hand and forearm fasciotomies. with carpal tunnel release.
Patient: 47-year-old male.
Presentation: Patient agreed to external tissue expansion reconstruction to diminish the wound size. Fasciotomies were performed. DERMACLOSE tissue expanders were applied to the wound.
Vac use: Yes
Outcome: 2 weeks post-operative the sutures were removed and the wound went on to complete healing. Skin-grafting was avoided thanks to external tissue expansion. Patient recovered the majority of his upper extremity function through occupational therapy.
Photos courtesy of Ajul Shah, MD
55-year female patient suffers soft tissue necrosis after right knee replacement
Injury: Soft tissue necrosis in right knee following right knee replacement surgery. Injury was caused due to poor access design of the incision.
Patient: 55-year-old female
Presentation: Soft tissue reconstructive options were contemplated. Soft tissue expansion was found to be the best solution due to deformity concerns related to skin grafts. Two dermaclose external tissue expanders were placed for expansion and were placed for wound closure.
Size of Wound: 20 cm x 12 cm
Vac use: Yes
Outcome: 2 weeks after post-operative sutures were removed and the wound was completely healed. Flap reconstruction of the knee allowed for the salvage of the implant, and the expanded and reconstructed donor site allowed for linear closure, preventing a large deformity of the leg.
Plastic surgery
Injury: Infected sternal wound resulting from oncologic excision
Surgeons: George Zorn, MD, Gregory Muehlebach, MD
Patient: 40-year-old male
Presentation: Patient came from an outside hospital with metastatic papillary thyroid cancer requiring further resection, radical neck dissection, and a redo of a sterotomy due to sternal wound infection with C. koseri .
Size of wound: 26 cm x 9 cm x 5.5 cm
Time to closure: 7 days
Vac use: Yes
Outcome: At his 6 week follow up patient maintained full closure and required no further follow up.
Injury: Dehiscence on the scalp vertex.
Surgeon: Bryan Cicuto, D.O.
Patient: 35-year-old female
Presentation: A 35-year-old female patient presented with a 3-month-old dehiscence on the scalp vertex after rotational flap treatment of basal cell carcinoma.
Size of wound: 6 cm x 3 cm
Time to closure: 5 days
Vac use: No
Outcome: At 3 month visit, sensory disturbance related to initialbrotational flap improved and the scalp wound was fully healed.
Injury: Necrotizing fasciitis of the left foot
Surgeon: Andrew G. Silver, MD, et al.
Patient: 55-year-old diabetic male
Presentation: Diabetic male patient presented with necrotizing fasciitis of the left foot and leg. After the infection was eradicated, a large soft tissue deficit was present on his foot and leg.
Size of wound: 40cm x 12cm
Time to closure: 7 days
Vac use: No
Outcome: Examination at week 5 revealed a stable, closed wound that is healing well.
Injury: Atopic dermatitis and squamous cell carcinoma of the upper back
Surgeon: Dr. Robert G. Chandler, MD
Patient: 50-year-old male
Presentation: The patient presented with atopic dermatitis and a large, poorly differentiated squamous cell carcinoma of the upper back. The carcinoma was excised resulting in a 15cm x 16cm deficit.
Size of wound: 15cm x 16cm
Time to closure: 2 days
Vac use: No
Outcome: At follow-up 6 weeks later, the wound had healed nicely
Injury: Breast reduction/mastopexy and liposuction of the lateral chest wall
Surgeon: Dr. David Azouz, MD
Patient: 46-year-old female
Presentation:The patient underwent breast reduction/mastopexy and liposuction of the lateral chest wall. Two weeks after the surgery the incision on the left breast dehisced due to poor wound healing as a result of chronic Epstein Barr virus with high viral load.
Size of wound: 6 cm x 3 cm.
Time to closure: 6 days
Vac use: No
Outcome: This case illustrates the successful use of DermaClose to accelerate and improve healing following dehiscence in breast surgery.
Injury:
25 year old male
Presentation: Patient was seen as a follow up after excision of a right thigh lesion. Unfortunately, the pathology showed Dermatofibrosarcoma
Protuberans, necessitating a wide local excision.
Size of wound: ~10 cm x 8 cm
Time to closure: 7 days
Vac use: No
Outcome: During follow up on post-operative day seven the leg looked good and the wound was well approximated. The patient was seen again two months later and was very satisfied with the results.
56 years old male patient
Presentation: Open abdominal wall defect
Size of wound: 32 cm
Time to closure: 5 days
Vac use: Yes
Outcome: Complete healing abdominal wall. Case demonstrates potential advantage of BOTOX administration in conjunction with tissue expanding capabilities of the DermaClose for managing challenging open abdomen cases.
53 year old male patient
Presentation:The patient was brought to the operating room the evening of presentation for evacuation of the extensive abscess, wash- out and placement of a wound VAC. The resulting 18 x 10cm wound could not be closed primarily and treatment options included prolonged VAC treatment
with subsequent split thickness skin graft.
Size of wound: 10 x18cm
Time to closure: 4 days
Vac use: Yes
Outcome: Follow up at six weeks from definitive closure shows the wound healing nicely with no complications.
56 years old male patient
Presentation: morbidly obese
male patient with multiple medical comorbidities including diabetes, renal insufficiency, atrial fibrillation, and Ogilvie’s Syndrome presented with a large ventral hernia and obstipation. He underwent a partial colectomy and ventral hernia repair.
Size of wound: 20cm x 20cm.
Time to closure: 8 days
Vac use: Yes
Outcome: : Post-operatively the patient did well and was discharged on post-op day 3 after the incisional VAC was removed and the closure was noted to be stable. The patient’s condition continued to improve and he was seen seven months post-closure with the wound still intact.
16 years old female patient
Presentation: Olecranon fracture with necrosis and split thickness skin grafting of the antecubital wound.
Size of wound: 8 x 8 cm with tethering to muscle
Time to closure: 4 days
Vac use: No
Outcome: Nearly 95% of the graft was excised. Patient is extremely happy with aesthetics and improved function.
44 year old gentleman
Presentation: Insulin dependent diabetes mellitus, MRSA, transverse myelitis and paraplegia. Patient also suffered multiple sacral and lower extremity pressure ulcers. Patient underwent split thickness skin grafting to the large extremity wound which ultimately failed.
Size of wound: 15x5cm
Time to closure: 4 days for left side of wound, 11 days for right side.
Vac use: Yes
Outcome: At 60 day follow up wounds continue to be closed and healing well.
14 year old male patient
Presentation:The patient was found to have a frontal sinus malignancy which was a desmoplastic small round cell tumor. He had a resection and reconstruction with autologous bone and required postoperative radiation and chemotherapy. He developed infection and spontaneous drainage of purulent fluid.
Size of wound: ~2cm
Time to closure: 6 days
Vac use: No
Outcome: The patient was seen two months after initial placement of Dermaclose. The incision closed completely and healed well with no fluctuance.
General surgery
Photos courtesy of J. Codd, MD
38 year old male patient
Presentation: ‘Deep Vein Thrombosis’ (DVT) which resulted in Compartment Syndrome, necessitating a Fasciotomy of the lower right leg.
Size of wound:35cm x 20cm
Time to closure: 9 days
Vac use: Yes
Outcome: The wound was dressed in the usual fashion and the patient returned to the OR three days later. The wound edges had fully approximated and the DermaClose devices were removed.
53 year old patient
Presentation: He had presented three days earlier when a large basal squamous cell carcinoma of the nose was removed.
Size of wound: 6 x 8cm
Time to closure: 6 days
Vac use: No
Outcome: At three weeks the patient returned for division and in-set of forehead flap to the nose. The flap donors site has healed
nicely and the patient is happy with the results.
60 y.o. female patient
Presentation: spontaneous bacterial peritonitis. She had a history of metastatic abdominal carcinoid. On 2/24 surgery was performed and the abdomen open due to and secondary to exploratory laparotomy with grossly infected peritoneal fluid.
Size of wound:14 x 6cm
Time to closure: 8 days
Outcome: The incision healed without incident and the drains were removed at one week following discharge. The patient was discharged six days after closure. At one month follow-up no breakdown or wound failure.
36 y.o. female patient
Presentation: Morbidly obese diabetic female patient originally presented with multiple incisional hernia in 2008. Hernias were treated with a succession of mesh products commencing with a non-biologic before progressing to a biologic mesh in Sept. 2009. Several weeks later in October 2009 a procedure was performed to remove a dermal collagen implant that had become infected.
Size of wound:28 x 23 cm
Time to closure: 9 days
Vac use: Yes
Outcome: Four month follow up. The patient returned in March 2010 for follow up. In that time a small wound of unknown origin had formed below the previously closed wound.
Foot and ankle surgery
A 42 year old African-American male
Presentation: presents to our clinic after stepping on a bottle cap in March 2007. The patient is a poorly controlled diabetic with serum glucose running between 250 and 350 mg/dL.
Size of wound:~10 x2cm
Time to closure: 3 days
Vac use: Yes
Outcome: The device is applied and within 3 days the dorsal defect closed.
63 y.o. male patient
Presentation: Type II diabetes and a recurrent ulcer under the right first metatarsal head. All symptoms of a serious diabetic foot infection. Skin perfusion pressures were >50 mmHg, ruling out significant peripheral artery disease.
Size of wound:2 x7cm
Time to closure: 5 days
Vac use: No
Outcome: After the plantar incision completely healed a 1st metatarsal phalangeal joint fusion was performed due to
the unopposed extensor hallucis longus to prevent recurrence of an ulcer.
48 y.o. male patient
Presentation: 430-pound diabetic male that sustained a left heel puncture wound from an unknown object while in New Orleans as a relief worker
following Hurricane Katrina in August of 2005. States his lower extremities were submerged for days at a time while continuing with the relief work.
Size of wound:3.6cm x 2.9cm x 1.2cm deep
Time to closure: One week
Vac use: No
Outcome: One week later the DermaClose was removed with 100% edge approximation. The skin edges were freshened and successfully closed without flap tension or suture ischemia.
68 y.o. patient
Presentation: poorly controlled diabetic that originally presented to the office complaining of a malodorous foot that was not responding well to 6
weeks of Vaseline on a dead plantar midfoot. The patient underwent revascularization and subsequent Chopart open amputation and VAC therapy.
Size of wound:3.8 cm x 8.5 cm x 2.5 cm
Time to closure: 7 days
Vac use: Yes
Outcome: The wound edges and granulation were freshened, and the wound was primarily closed without complication.
45 y.o. male patient
Presentation: presented with an abscess on the plantar aspect of the 1st metatarsal. He was admitted to the local hospital and on the same day
underwent an I&D procedure.
Size of wound:
Time to closure: Twenty four hours
Vac use: No
Outcome: He was discharged on hospital day #5 with strict instructions for non-weight bearing. Patient was subsequently seen in the office on
weekly basis. At six weeks post-op his incision site was 95% epithelialized with superficial gapping seen at the distal most aspect of the incision. In
this particular case the use of DermaClose allowed us to close the wound primarily (delayed) vs. allowing the wound to heal by secondary intention.
In addition, the patient left the hospital with a closed wound and less risk of developing a recurrent wound infection..
58 y.o. male patient
Presentation: Patient with diabetes mellitus who underwent partial first ray amputation that was left open. This was performed due to osteomyelitis of the first metatarsal.
Size of wound:4.0 x 2.5 cm x 1.5 cm deep
Time to closure: 24 hours
Vac use: No
Outcome: At one month status post delayed primary closure his wound is progressing well.
54 y.o. male patient
Presentation: Patient with Buerger’s disease and a non-healing ischemic ulcer to the dorsum of his left hallux for almost two years. He has a 30 pack per
year smoking history and quit a year ago. An angiogram performed in July of this year showed severe medium and small vessel disease of the left lower extremity.
Size of wound:7 cm
Time to closure: 4 days
Vac use: No
Outcome: The patient was returned to the OR 4 days later. The DermaClose device and skin anchors were removed and the wound site prepped and draped in usual fashion.
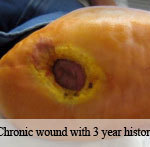
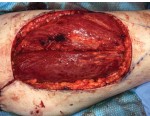
47 y.o. male patient
Presentation: Patient wit a past medical history significant for depression and recurrent left Achilles tendon ruptures, chronic wound to the left leg13 months duration and depression. S.B’s past surgical history was significant for three open Achilles tendon surgical procedures including primary repair of an acute rupture, delayed repair of the Achilles tendon with augmentation with an allograft and a flexor hallucis tendon transfer with left hallux interphalangeal joint arthrodesis.
Size of wound:10cm long x 3cm width
Time to closure: 4 days
Vac use: No
Outcome: The wound was further sutured closed and the device removed. The extremity was casted in a below knee gravity equines cast.
Photos courtesy of Ajul Shah, MD
A 27-year-old male suffers mid foot fractures and severe soft tissue destruction
Presentation: Patient suffered multiple mid foot fractures as a garbage truck rolled over and crushed his left foot. Soft tissue was debrided through multiple operations, eventually requiring amputation of two toes.
Size of Wound: 15 x 10 cm
Time to closure: 10 days
Outcome: After 2 weeks post-operative, the patient’s sutures were removed and the would completely healed. The patient’s free ALT flap reconstruction of the left foot allowed for limb salvage and a functional foot.
Vascular surgery
AAA repair in 43-year old male with multiple comorbidities
Presentation: Patient required AAA repair, presented with multiple comorbidities, including heart failure, diabetes, and obesity.
Size of wound: 7.8 cm
Time to closure: 5 days
Vac use: No
Outcome: At 6 weeks post DermaClose removal the patients had healed well with the exception of a small Keloid. The surgeon was very satisfied with the use of DermaClose.
Photos courtesy of Adam B. Levitt, MD
31 year old male
Presentation: Gunshot wound (GSW) to the left popliteal fossa. On exam the patient was found to have no palpable pulses in the left foot, with no sensation to touch and an inability to move the foot. X-ray revealed a comminuted distal femur fracture.
Size of wound: ~15 cm x 10 cm
Time to closure: 5 days
Vac use: Yes
Outcome: The medial wound was closed primarily but there was too much tension to close the lateral fasciotomy site. Dermaclose device was placed using the shoelace technique. The patient had no complaints of pain with the device in place.